Determinants of Patient Satisfaction in Post-LASIK Patients Undergoing Cataract Surgery
By Frank A. Bucci, Jr., MD
Post-LASIK patients have long been perceived as a challenging group when it is time for cataract surgery. As evidenced by their prior laser vision correction, these patients prioritize spectacle independence and may wish to have presbyopia-correcting IOLs implanted. However, achieving accurate IOL power calculations in these eyes is more difficult, and they also have a higher rate of higher order aberrations (HOA).
In a study presented at the 2020 virtual ASCRS meeting, I looked at visual outcomes and patient satisfaction in 61 post-LASIK eyes that underwent cataract surgery. Three cohorts were analyzed: Tecnis +3.25 Multifocal IOLs (Johnson & Johnson Vision ZLB00, n =3 2), Tecnis Symfony extended-depth-of-focus (EDOF) IOLs (n = 11), and monofocal IOLs, either a Tecnis aspheric monofocal or a Bausch + Lomb Akreos monofocal (n = 13). Using a multivariate regression model that I have previously used in three other studies, we looked at the relationship between 50 independent variables that were regressed against the dependent variable of “overall patient satisfaction”. The independent variables included 19 subjective variables related to the performance of common visual tasks, which were assessed by patient questionnaire. There were also 31 objective clinical metrics, such as visual acuity, residual sphere/cylinder, IOL centration, angle kappa, HOA, reading speed, and more.
For all 61 eyes across all three IOL cohorts, patients reported being very satisfied or satisfied for the dependent variable of “overall patient satisfaction”. However, a significantly greater percentage were very satisfied in the multifocal (90.6%, P = 0.007) and EDOF (81.8%, P = 0.011) groups compared to the monofocal group (30.8%).
As one might expect, some HOAs (RMS P = 0.009, coma P = 0.038, trefoil P = 0.049, and spherical aberration P = 0.011) in this group of 61 post-LASIK eyes were statistically significantly higher than the HOAs in a separate cohort of 350 eyes with no prior LASIK that had undergone cataract surgery with implantation of presbyopia-correcting IOLs.
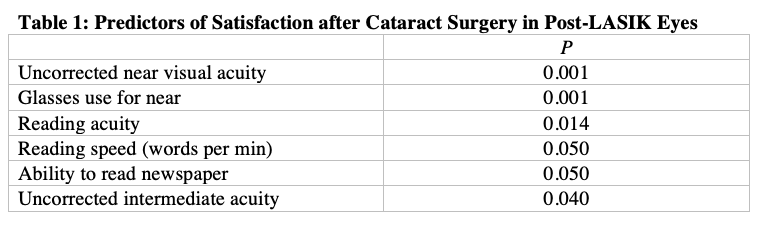
Regression analysis detected six out of 50 independent variables that contributed significantly to the patients’ decision regarding the dependent variable of “overall patient satisfaction.” As shown in Table 1, five of these variables were directly related to near vision, and one to intermediate vision.
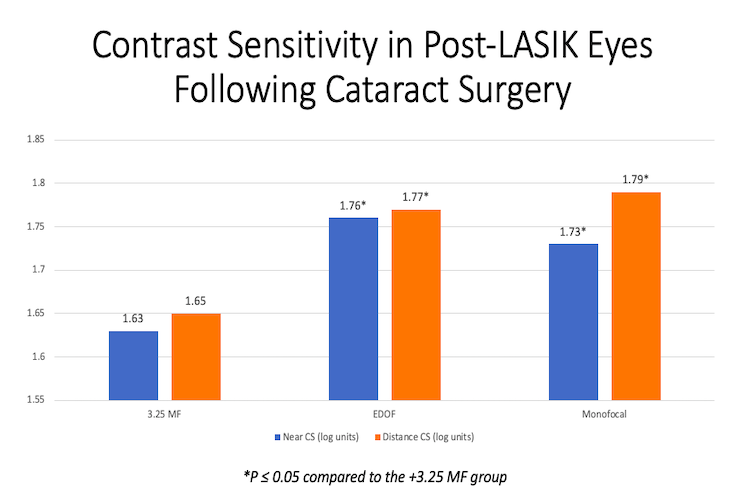
The EDOF and monofocal groups had better contrast sensitivity than the multifocal IOL group at both near and distance (Figure 1).
Interestingly, our regression analysis detected no statistically significant contributions to overall patient satisfaction from variables related to light phenomena at night, including halos, glare, and starbursts. In other words, patients’ satisfaction was not significantly dependent on whether they experienced these symptoms.
In conclusion, the +3.25D ZLB00 multifocal IOL evaluated in this study achieved the highest percentage of “very satisfied” patients and the Symfony EDOF group achieved high levels of “very satisfied” compared to those implanted with monofocal IOLs. The multifocal IOLs achieved these very high levels of satisfaction despite relatively high levels of HOAs (compared to non-post-LASIK eyes) and worse contrast sensitivity performance compared to the other types of IOLs. The multivariate regression strongly suggests that uncorrected near and intermediate vision are very important to post-LASIK patients.
Following proper patient selection, Tecnis +3.25 ZLB00 IOLs and Symfony EDOF IOLs are viable IOL choices and achieve high levels of patient satisfaction in post-LASIK patients undergoing cataract surgery. These findings appear to dispel the notion that this patient population can’t be successful with multifocal IOLs because of less than optimal contrast sensitivity, greater HOAs, or dysphotopsias at night. In actuality, the ability to meet the patients’ visual targets at all distances—and especially at near—strongly outweighs other factors in producing post-LASIK patients with high levels of patient satisfaction.
Dr. Bucci is the founder of Bucci Laser Vision Institute in Wilkes-Barre, Pa. He is a consultant to Bausch + Lomb and Johnson & Johnson Vision, and this study was funded by Johnson & Johnson Vision. Contact him at (570) 825-5949 or [email protected].