The Impact of Nocturnal Blood Pressure on Normal-Tension Glaucoma
Experts acknowledge that patients with normal-tension glaucoma (NTG) are a challenge to manage. Since low-blood pressure (BP) is associated with prevalence and incidence of glaucoma, getting a handle on BP in patients with NTG is imperative. Until recently, most studies have measured pressure in such individuals during the daytime and usually only once or twice a day. Additionally, some study results suggest paying most attention to systolic BP, whereas others recommend monitoring diastolic pressure. But what’s the ideal? And where do nocturnal values come in?
Junki Kwon, an ophthalmologist from the College of Medicine at the University of Ulsan, Asan Medical Center in Seoul, South Korea, said he thinks more attention should be paid to nighttime BP—specifically, nocturnal diastolic BP. He bases this assertion on the results of a retrospective, longitudinal study involving 119 individuals. Participants averaged 54 years of age and were followed for an average of approximately 40 months, during which time 5 or more visual field tests were administered.
At baseline, investigators took 24-hour ambulatory BP measures (nocturnal and diurnal) and recorded intraocular pressure (IOP). They also measured nocturnal BP dip, using systolic and diastolic BP variables according to these 3 units:
- Percentage, which represented the degree at the risk point of BP (this cut-off value was BP >10 mmHg below daytime average BP).
- Time, which represented how long BP was below the risk point cut-off value.
- Area, which represented the duration and degree of the BP dip below the cut-off value.
For BP parameters, average, peak, trough, and range of systolic and diastolic BP during day and night were analyzed separately as independent variables.
Forty-one patients experienced visual field (VF) progression; the rest remained VF stable. Approximately, 1/3 of patients with VF progression developed optic disc hemorrhage versus 14% of those who remained VF stable. Visual field index progression rate was approximately 3.2% and -0.7%, respectively. Patients with VF progression were taking an average of 1.6 glaucoma eyedrop medications versus 1.0 for those who were VF stable.
Significant Nighttime Differences
Regarding BP levels, Dr Kwon’s team observed statistically significant nighttime differences between patients with VF progression and those who remained stable, whereas daytime readings were similar in both groups. Specifically:
- Nighttime average systolic BP levels were 108.9 mmHg and 114.9 mmHg, respectively.
- Nighttime diastolic readings were 68.3 mmHg and 73.9 mmHg, respectively.
- Daytime averages for systolic and diastolic were similar in the 2 groups.
- Nighttime trough systolic readings were 98.9 mmHg and 107.5 mmHg, respectively.
- Nighttime trough diastolic readings were 57.2 mmHg and 63.9 mmHg, respectively.
- Daytime trough levels for systolic and diastolic were similar in the 2 groups
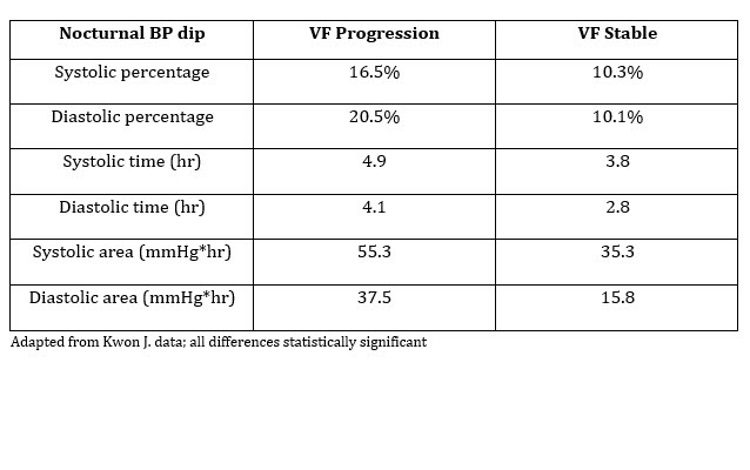
Meanwhile, nocturnal BP dip was significantly greater in patients with VF progression in all 3 units measured: percent, time, and area (see accompanying table). However, none of the diurnal BP variables were significantly different between the 2 groups. Nighttime and daytime IOP parameters were also similar.
In univariate analysis of systolic and diastolic nighttime trough levels, nocturnal BP dip percent and time were significantly associated with VF progression. “However,” noted Dr Kwon, “in a pairwise comparison….diastolic BP parameters had a greater association with visual field progression than systolic BP parameters.”
Meanwhile, in multivariate analysis, diastolic nighttime trough BP and BP dip area was significantly associated with VF progression. No systolic BP parameters were linked with progression.
An Additional Modifiable Risk Factor
Dr Kwon noted that ophthalmologists should be giving “greater attention to diastolic BP at night. Nocturnal diastolic BP dip may have a greater impact on NTG diseases progression than systolic.” Furthermore, “diastolic nocturnal BP dip should be considered as an additional modifiable risk factor for NTG eyes with visual field progression despite well-controlled IOP.”
From a practical standpoint, Dr Kwon noted that excessive nocturnal BP typically presents in 2 ways: Patients who are taking antihypertensive medications, and those who are not. For individuals in the first group, he advised talking with the patient’s primary care clinician about the possibility of less aggressive treatment. For those in the second group, “anecdotal data suggests that we can think [about] exercise, increased hydration, and/or nighttime salt intake.” Here, too, it is important to coordinate with the primary care clinician, since adjusting salt intake can impact other chronic conditions the patient may have. This is especially true for older individuals.
While some studies have observed lower nocturnal BP mostly in patients taking antihypertensive medications, Dr Kwon noted that in his study, his team observed that even those not taking such meds can still develop primary vascular dysregulation.
Kwon J. Which is most relevant to visual field progression in normal-tension glaucoma? Systolic vs. diastolic and daytime vs. night-time blood pressure. Talk presented at: AAO 2018 annual meeting; October 26-30, 2018; Chicago.