iAccess: A Novel Goniotomy Tool for the Reduction of Intraocular Pressure
By Mark Gallardo, MD and Matthew Porter, MD
iAccess is a new micro-invasive glaucoma surgery (MIGS) instrument designed to enhance aqueous outflow by manipulating the proximal portion of the conventional outflow system—the primary site of increased pathological flow resistance in eyes with open angle glaucoma. iAccess is a single-use circular blade (30-gauge, titanium-nitride coated) that has the flexibility to incise and excise the trabecular meshwork (TM) and inner wall of Schlemm’s canal (SC) (Image 1a, b) in multiple ways, providing surgeons with the novel ability to adjust their goniotomy procedures to meet the individual needs of each patient. The device has a 300-µm-deep built-in safety backstop and is made with an ergonomic, custom-tapered handle.

One of the goniotomy methods enabled by iAccess is to utilize multiple incisions that excise 220-micron segments of the diseased trabeculum to create an extensive opening over multiple clock hours. The objective of this goniotomy procedure is to enhance outflow from the anterior chamber to Schlemm’s canal, collector channels, and distal outflow system, which is similar to other goniotomy procedures using direct visualization while using a gonio lens. Moreover, iAccess can preserve significantly more tissue as compared to other procedures available today, helping to maintain the blood-aqueous barrier and the physiological, pulsatile pumping mechanism of TM/SC complex that facilitates aqueous outflow.1 Also, the surgeon is unrestricted in the number of excisions made or the clock hours treated, thereby creating an extensive opening to Schlemm’s canal. The versatility of the procedure allows iAccess to be used as a standalone procedure or combined with other technologies and utilizes the established category 1 CPT code 65820.
Micro-invasive glaucoma surgery (MIGS) offers the ability to lower intraocular pressure along with an excellent safety profile. They may also help reduce the glaucoma medication burden that can have troublesome side effects for patients, impacting quality of life and adherence concerns. One such MIGS, iStent inject W combined with cataract surgery, has commonly been utilized to successfully lower intraocular pressure with a relatively low risk of significant complications.2 Clinical trials with the iStent brand of trabecular bypass stents, spanning 5 years or longer, have confirmed the long-term benefits of intraocular pressure and medication reduction.3 Large landmark trials (Early Manifest Glaucoma Trial and Ocular Hypertension Therapy Study)4,5 have demonstrated that lowering IOP by 1 mmHg may reduce the risk of glaucomatous progression by 10%. Looking at the use of multiple iStents in comparative studies, there is ample evidence of a dose response with an increasing number of iStents corresponding to a progressively lower postoperative IOP.6,7 Used in conjunction with iStent inject W, iAccess may further lower intraocular pressure by creating an extensive opening of the trabecular meshwork, while leaving 2 iStent inject W stents in place for a long-term, permanent bypass.
Clinical Trial and Data
This non-randomized, observational case series of procedures from multiple surgeons compared outcomes of 2 subgroups:
- Group A (n = 63 eyes) cataract extraction with intraocular lens placement and iStent inject W
- Group B (n = 92) cataract extraction with intraocular lens placement with iStent inject W plus iAccess goniotomy.
In all cases, 2 iStent inject Ws were successfully implanted. In group B, iAccess created incisions and excisions across the trabecular meshwork spanning more than 90 degrees. Patients were monitored for 3 months (evaluation ongoing) noting the intraocular pressure and the number of glaucoma medications. With the exception of occasional and self-limiting micro-hyphema, there were no complications noted.
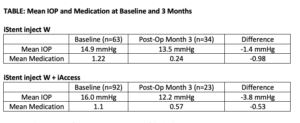
At 3 months, Group B (iStent inject W + iAccess) had a lower post-op mean IOP at 12.2 mmHg versus 13.5 mmHg for Group A, resulting in an impactful and substantial difference of 1.3 mmHg. The addition of iAccess goniotomy in Group B also enabled a higher percentage of eyes to reach a target intraocular pressure of below 15 mmHg (91.3% vs 76.5% in Group A). Both groups had a high percentage of eyes that remained glaucoma medication-free at 3 months (80-85%).
The versatility of the iAccess procedure allowed for additional IOP reduction when paired with iStent inject W by synergistically providing further reduction in outflow resistance while maintaining an excellent safety course. The encouraging results seen in these patients enrolled in this initial surgical series need to be followed for long term outcomes. In addition, further data collection is ongoing to help confirm the benefit of pairing iStent inject W trabecular bypass surgery with iAccess goniotomy. iAccess introduces another attractive MIGS surgical option that offers hope in improving the care of glaucoma patients by helping to maintain their vision by maintaining an ideal intraocular pressure and limiting the need for medications. iAccess provides an elegant, less destructive method for precise trabecular goniotomy that may be paired with other MIGS procedures as deemed medically necessary by the surgeon. This pairing of 2 MIGS procedures (with favorable benefit-to-risk ratios) using 2 different devices with 2 separate indications provides one possible novel way of additional IOP reduction to lessen the glaucoma drug burden in patients where surgeons prefer to avoid riskier glaucoma operations.
Reference
- Johnstone MA. The aqueous outflow system as a mechanical pump: evidence from examination of tissue and aqueous movement in human and nonhuman primates. J Glaucoma. 2004;13:421-438.
- Samuelson, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126:811-821
- Hengerer FH, Auffarth GU, Conrad-Hengerer I. iStent inject Trabecular Micro-Bypass with or Without Cataract Surgery Yields Sustained 5-Year Glaucoma Control. Adv Ther. 2022;39(3):1417-1431. doi: 10.1007/s12325-021-02039-4.
- Leskea MC, Heijl A, Hyman L, et al. Factors for progression and glaucoma treatment: The Early Manifest Glaucoma Trial. Curr Opin Ophthalmol. 2004 Apr;15(2):102-6. doi: 10.1097/00055735-200404000-00008.
- Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701-13; discussion 829-30
- Katz LJ, Erb C, Carceller A, et al. Prospective, randomized study of one, two, or three trabecular micro-bypass stents in open-angle glaucoma subjects on topical hypotensive medication. Clin Ophthalmol. 2015;9:2313–2320.
- Popovic M, Campos-Moller X, Saheb H, Ahmed IIK. Efficacy and Adverse Event Profile of the iStent and iStent Inject Trabecular Micro-bypass for Open-angle Glaucoma: A Meta-analysis. J Curr Glaucoma Pract. 2018;12(2):67-84. doi: 10.5005/jp-journals-10008-1248. Epub 2018 Aug 1. PMID: 30473602; PMCID: PMC6236117.

