Patient education strategies boost compliance with dry eye disease management
By Mark E. Schaeffer, OD, FAAO
When patients come into the practice for an annual exam and new glasses, they’re not typically expecting a dry eye disease (DED) diagnosis. This can trigger another visit, more tests, and multiple therapies, and many of my patients have this very experience. Fast forward a few months after their initial visit, and they’re using the therapies I rely on for DED management, such as a nutraceutical (HydroEye, ScienceBased Health) and preservative-free artificial tears (iVIZIA, Thea), with the possible addition of a prescription therapy such as cyclosporine or lifitegrast (Xiidra, Bausch + Lomb) or an in-office therapy like thermal expression (TearCare, Sight Sciences).
How can we help patients take the journey from a routine refractive visit to managing their DED every day? Education is the key. To make sure DED education connects and resonates throughout this process, lay the groundwork with concrete diagnostic data, focus on the patient’s perspective, and always explain the reasons behind your therapeutic choices to gain compliance.
Lay the groundwork with diagnostics
For education to resonate strongly with patients, it has to be tangible. The first basis for that tangible connection is to share what I see in their screening and testing.
For screening, I follow a 2-step process. First, all patients get a brief DEQ-5 (dry eye questionnaire). If they score 6 or higher, I discuss their DED symptoms. My second step is to observe patients at the phoropter. Most patients with DED have occasional blurry vision, eye fatigue, trouble driving at night, or nonspecific visual symptoms (eg, “I’m not seeing as well as I normally do, even with my glasses on.”). If, when they get behind a phoropter and I ask, “Which is better, 1 or 2?” and they blink to clear their vision, that’s it for me—they have DED.
Once I’ve identified DED, educated the patient, and initiated over-the-counter treatment (nutraceuticals and/or drops), I book a medical visit, where additional tests include fluorescein and lissamine green staining, meibography, osmolarity, and inflammatory markers. Beyond their diagnostic value, these test numbers and images go a long way to support patient education.
Below are some best practices and pearls that I have used to best educate my patients with DED.
Teach to the patient’s perspective
When patients find out they have a condition, they want to feel reassured, get easy-to-understand explanations, and be shown a clear treatment path.
Use the term “ocular surface disease.”
We’ve all told patients, “You have dry eyes disease” and had them respond, “My eyes aren’t dry—they’re watery [or itchy or blurry],” after which we say, “Yes, but that’s because they’re dry…” Rather than start on a circuitous and confusing path like this, I like to proactively educate the patient. I use the broader term “ocular surface disease” rather than DED and explain how it is affecting their vision, drawing on specific test findings.
For example, I might tell a patient, “You scored pretty high on the questionnaire you filled out, so it doesn’t surprise me that you’re having some vision fluctuation. Based on your feedback and what I saw in your exam, you have a condition called ocular surface disease. It’s very common. It means that your tears don’t work as well as they should. This is treatable, and we have a lot of options to help.”
State the next steps.
Lay out their next steps at every visit. For example, once screening shows a patient has DED, I might say, “Now that we know you have ocular surface disease, we’re going to bring you back for another visit where we can see what the ocular surface looks like, do some quick tests, and then go through the results to determine your best treatment.”
Turn tests into teaching aids.
Meibography, staining, osmolarity, and MMP-9 (Matrix Metalloproteinase-9) testing are all concrete ways to educate patients about DED and get buy-in. I often tell patients, “Here’s what your clogged oil glands look like, and here’s what normal glands look like.” If osmolarity and MMP-9 numbers are off, I explain, “This number shows that you’re not making the right concentration of tears, and you’re positive for inflammation, which tells me that a prescription medication may work best for you.”
Explain therapies to ensure compliance.
To ensure that patients adhere to the specific name brands I recommend, I explain, “The surface of the eye is very delicate and sensitive, so we need to be careful about what we put on it. I’m specifically recommending iVIZIA artificial tears because they’re preservative-free, so we’re avoiding some ingredients that can cause irritation, and they work very well for my patients with this problem.” Recently, patients have seen the headlines about eye drop contamination and FDA recalls, furthering their hesitation to use generics. When patients understand why I choose a specific drop, they see it is important to follow instructions and not buy a lesser alternative.
Education challenge: DED with toxic maculopathy
A 72-year-old woman had toxic maculopathy caused by an oral medication, causing her vision to slowly worsen over time and reach 20/100 in her right eye, but she still had the functional vision to read and do normal activities. I had been watching this condition for 5 years when she reported to the clinic with foreign body sensation, swelling, irritation, and tearing in the right eye. She complained of blurred vision that would not resolve, which was especially frustrating because she was already visually compromised. She had difficulty reading. I explained to the patient, “Your symptoms point to ocular surface disease, which is common and treatable. Let’s do some tests to find out the best way to get you feeling better.”
The patient had 3+ fluorescein staining from the central cornea to the inferior limbus in the right eye, indicating superficial punctate keratopathy. The inflammatory nature of the condition warranted a steroid, but due to the central nature of the condition, I added a lubricating drop. I showed her the staining and told her, “The areas that are lit up here are where cells on the surface have become damaged. We’re going to clear that up and stop the inflammation with a steroid eye drop, which you’ll use 4 times per day. To help that area heal faster and help you feel more comfortable between the steroid eye drops, I’m also prescribing a preservative-free artificial tear called iVIZIA that I want you to use every hour.”
When the patient returned 2 weeks later after taking loteprednol (Lotemax, Bausch + Lomb) and iVIZIA, her vision and corneal staining were back to pre-episodic levels. She felt good about her vision. Her eyes felt much better without the irritation and wildly fluctuating vision. The steroid drop was discontinued, but I explained, “I want you to stay on this specific brand of eye drops twice per day to continue providing the lubrication you need to feel comfortable and prevent superficial punctate keratitis from happening again.” By educating the patient about this complex situation, I was able to reassure her and help her continue getting the therapy she needed.
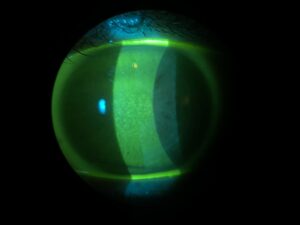
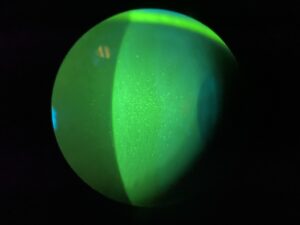
Caption: The patient’s fluorescein staining shows superficial punctate keratopathy.
Mark Schaeffer, OD, FAAO, earned his Doctor of Optometry from Southern College of Optometry and completed a residency in Ocular Disease at Bascom Palmer Eye Institute in Miami, FL. He serves as Clinical Field Manager at MyEyeDr in Birmingham, AL, where he practices full-scope optometry. He is affiliated with several pharmaceutical companies in consulting for ocular disease and contact lenses. Disclosures: Bausch + Lomb, ScienceBased Health, Sight Sciences, and Thea.

