Playing the Glaucoma Game
By Savak “Sev” Teymoorian, MD, MBA
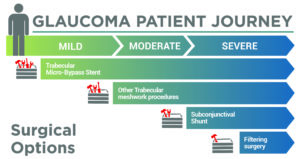
When I see a new glaucoma patient, we begin a lifelong journey together. Our goal is to get to the end of life with good, functional vision. No one knows how long this journey is going to be, how quickly disease will progress, or how long the lifespan will be. When we run into those inevitable obstacles, I want to have the maximum number of tools available to me in an effort to overcome each one. Thus, there is an optimal treatment selection order to maximize the possible number of future treatments, and it is my goal to make these selections in the most strategic manner.
With this in mind, the first surgical step to treating glaucoma is in the trabecular meshwork with a bypass device. A trabecular bypass, like an iStent inject W (Glaukos Corporation), allows me to maintain all other glaucoma treatment options for the future, or the greatest number of tools still in my toolbox to choose from. Although some may feel that a goniotomy is a similar first step as it works in the same space, a goniotomy results in the removal of tissue. This eliminates the possibility of later implanting a trabecular bypass stent or future devices that may need to be implanted in the trabecular meshwork, including sustained-release drug eluting devices that are currently in clinical trials. On the other hand, if you insert a stent and later feel that more intraocular pressure (IOP) lowering is needed, it is still possible to perform a goniotomy or other procedure.
ld still combine cataract surgery with an iStent, particularly now that it comes with 2 wide-flange stents for a significant degree of IOP reduction. I can always return and perform a goniotomy as a stand-alone procedure later. I am lining up my procedures to keep as many options as possible for the remainder of the continuing care journey and in consideration of the most beneficial treatment plans for my patients.
If a patient has a cataract, even if their glaucoma is fairly advanced, there is no reason not to combine cataract surgery with a MIGS procedure. As disease becomes more advanced, with IOP in the high 20’s or even 30’s, lesser invasive options can still be used. I wou
The FDA approval of this stent further strengthens the risk-to-benefit ratio of MIGS devices. This device offers the added benefit of a wider stent flange, which optimizes visualization while maintaining a truly microscale footprint, and significantly enhances predictability in stent placement. With 2 stents contained in a single injector that are deployed approximately 2-3 clock hours apart, it provides significant IOP reduction while maintaining a similar risk profile as cataract surgery alone.1
As a patient progresses in their disease after receiving a trabecular bypass, my next step is goniotomy. For example, the Kahook Dual Blade (New World Medical) removes a section of the trabecular tissue without violating the scleral wall or creating a bleb. The ab interno procedure gives aqueous direct access to the collector channels and the distal outflow system be used as a standalone procedure or in conjunction with phacoemulsification.2
When it becomes necessary to advance a step in treating a patient’s glaucoma, my next move will be to the subconjunctival space. The XEN Gel Stent shunts fluid from the anterior chamber to the subconjunctival space, creating a low, diffuse bleb. The procedure bypasses the normal drainage pathways and thus is able to produce low IOPs in refractory, diseased eyes. The device is indicated for refractory glaucoma and while the procedure is more invasive than an iStent, and has a greater degree of associated risk, it is still highly preferable to a trabeculectomy or tube shunt and in some cases is able to provide similar IOP-lowering capability.3
Trabeculectomy and tube shunts are my last step. They are highly effective at providing a dramatic lowering of IOP and very useful, but they also bring many risks, some of them sight-threatening. Thus, while these options are definitely on my game board, they are at the end.
The better prepared I am as a glaucoma specialist and the more well-versed I am in the variety of treatment options available, the better I can design an appropriate path for my patient. Chronic diseases are managed, not cured. Although we all know this, we still tend to be drawn to ‘blockbuster’ treatments that appear as if they will give us the greatest impact with the least follow-up, but it rarely happens this way. This is an exciting time to treat glaucoma with a plethora of therapeutic options. If we use them wisely, we preserve the greatest number of tools for our patients’ future needs.
Savak Teymoorian, MD, MBA, is a cataract and glaucoma specialist at Harvard Eye Associates located in Orange County, CA. Dr. Teymoorian can be reached at 949-951-2020.
Reference
1. Samuelson TW. Prospective, randomized, multicenter clinical investigation of the Glaukos iStent inject. Presented at: American Society of Cataract and Refractive Surgery annual meeting; April 13-17, 2018; Washington.
2. Abdullah S, Jasek MC, Radcliffe NM, et al. A novel dual blade device for goniotomy: initial clinical experience. Invest Ophthalmol Vis Sci. 2016;57(12):6522.
3 Galal A, Bilgic A, Eltanamly R, Osman A. XEN glaucoma implant with mitomycin C 1-year followup: results and complications. Journal of Ophthalmology 2017. Article ID 5457246, 5 pages.
